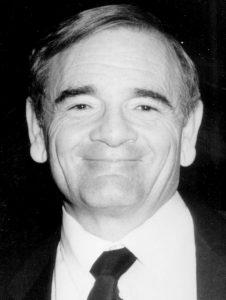
Professor Stanley Shaldon was born in 1931 in London to immigrant Sephardi Jewish parents. The family name was changed from Schlaff to Shaldon in 1943 as a consequence of the Second World War, during which he was a runner for the Air Raid Protection service.
Stanley Shaldon was an unorthodox figure, but had a brilliant academic career and was a major figure in Nephrology and especially hemodialysis for many decades, introducing and promoting new ways of treating patients with renal failure.
Stanley’s education commenced at University College School, Hampstead where the twin principles of freedom of intellect and respect of individuality were prized. He exercised these principles to the full extent.
Finishing school at age 15 years, he studied at the Sorbonne in 1949 [Cours de Civilisation Française]. He won an exhibition to Queens College, Cambridge to study medicine (1949-1952) and took additional courses in experimental psychology. At Cambridge he played for the Freshman Rugby and water polo teams.
His clinical instruction was at the Middlesex Hospital (1952-1955) where he received the majority of awards given for the best student of the year. Including the postgraduate prize in applied pharmacology, the second Broderip scholarship, the John Murray scholarship and gold medal in theoretical and Practical medicine, and the Hetley Clinical Prize in Medicine, surgery and obstetrics.
After training in Internal Medicine at the Middlesex Hospital and Hammersmith Hospital [Royal Postgraduate Medical School], he spent 2 years [1957-1959] in military service as a Medical Specialist at a military hospital in Lagos, Nigeria and published papers on Tropical diseases.

On his return from Africa, Dr Shaldon worked from 1959-1960 as a Registrar at the Royal Postgraduate Medical School, where he learned vascular catheterization techniques with Professor Sir John McMichael [Munk’s Roll, Vol.IX, p.341]. He also worked with Professor Dame Sheila Sherlock [Munk’s Roll, Vol.IX, p.514] commencing his thesis on the splanchnic circulation, which won the Raymond Horton-Smith prize and a Gold medal at Cambridge University in 1961.
In 1957 he passed MRCP and 1981 was elected FRCP.
In 1960 Dr Sherlock moved to the Royal Free Hospital to become the first full time female Professor of Medicine in the UK .She appointed Stanley Shaldon as Lecturer in Medicine. She noted the paucity of interest in Nephrology and delegated Stanley to form a renal division in 1960. The clinical service was deeply involved in the management of Acute Renal Failure. Research in this subject was intensively pursued with regard to pathophysiology, including measurement of renal blood flow and renal metabolism. The effect of increasing frequency of dialysis in reducing morbidity and mortality was noted and recommended. This observation required increased and economic use of dialyzers resulting in the establishment of a program for dialyzer reuse, and designs of new methods of continuous vascular access. Shaldon designed and personally made catheters which remained in situ in the femoral vein so that daily dialysis could be performed. It was noted that slow dialysis caused less complications. Neurological problems associated with dialysis were investigated and controlled, as described in the publication of Dialysis Disequilibrium Syndrome.
A typical work day would consist of patient rounds at 06.30 am, then starting patient dialyses, followed by visiting warehouses in London to obtain materials to construct vascular access catheters. This was done without the assistance of biomedical services. An invitation was given by the RSM to present these data in 1961.
Shaldon arranged a seminal symposium on Acute Renal Failure at the Royal Free Hospital in 1963, with participation by nephrologists from Europe and North America. He co-edited the proceedings.
At this meeting he discussed the concept of founding a European Dialysis and Transplant Association with Drs Willem Druckker and David Kerr [Munk’s Roll, Vol.XII, web]. He played an important role in the subsequent development of this organization, and later received its highest awards as Honorary Member, a life achievement certificate, and then the creation of the Stanley Shaldon Young Investigator Award.
With the development of long-term vascular access in the form of femoral venous catheters, chronic haemodialysis was begun at the Royal Free Hospital in the Spring of 1961, for the first time outside Seattle, and results were published in the proceedings of the International Congress of Nephrology in Prague in 1963. His interest grew in providing the service on a routine basis, and he pioneered self- home and overnight dialysis in 1964. He joined Professor Hugh de Wardener [Munk’s Roll, Vol.XII, web] in persuading the Department of Health to set up routine facilities for dialysis in the NHS.
In 1965 he was appointed Consultant Physician in the Renal Unit at the Royal Free Hospital but his quest for independence and diversity led to his departure in 1966 when he set up the National Kidney Center in an ordinary house to treat and train patients and their families in the techniques of haemodialysis at home. During his intensively productive period at the Royal Free Hospital his many co-workers included Stanley Rosen, Angus Rae, Rosemary Baillod, Chris Comty, and Felix Konotey-Ahulu.
His subsequent successes proved that his concepts were correct. He not only installed many patients in the home both in the UK and various other places throughout the world, but in addition established training centres in Germany, at university clinics in Frankfurt, Gőttingen and Hannover, and decisively contributed to the establishment of the nationally-important Kuratorium fűr Hemodialyse in 1970. In 1974, he was awarded a Visiting Professorship at the University of Montpellier, in France, working with Charles Mion. From 1976–1977 he was a visiting scientist at St Eric’s Hospital Stockholm where he worked with Drs Jonas Bergstrőm and Peter Furst. In 1977 he was responsible for the research section of department of nephrology at the University Hospital in Nimes.
Subsequently he became interested in the characteristics of ultrafiltration. He cooperated with Charles Dinarello and Lee Henderson in relating interleukin-1-mediated pathologies with hypotension, fevers and other complications during hemodialysis possibly associated with dialysis membranes. Latterly he had become a strong advocate for reduction of dietary sodium and control of anemia in chronic dialysis patients.
In a video interview, Shaldon described the pioneering years of dialysis and his own clinical and scientific philosophy.
Dr Shaldon was generous with his time and friendship and in his personal relationships showed deep sensitivity. However, he had a complex and enigmatic approach to academic discussion.
One of us has described elsewhere academic interaction with him: ‘no-one who met him will ever forget Stanley Shaldon. His manner was direct, dominant, and aggressive. On the other hand he had a good sense of humour. He had no qualms about offending people, and even went out of his way to do so. It was as though he was testing you out to see just how much you could stand. He was a sworn enemy of pomposity, cant and any sign of afflatus. On the other hand he defended and at times overestimated both in word and in print his own position, standing and contribution, even though there was never any need for this. To turn Churchill’s aphorism on its head, he was an immodest man with much to be immodest about.’
Professor Shaldon had a lifelong interest in developing equipment for medical research and therapy. He designed and manufactured Dylade equipment and influenced and cooperated with multinational manufacturers in the development of dialysis equipment. Herman Goehl of Gambro AG wrote ‘Stanley was a great person. He contributed so much for the development of hemodialysis. He stimulated and encouraged scientists, clinicians and technicians. I remember many big events he has influenced’.
He is survived by his wife, Penelope, and a son and daughter by a previous marriage.
[European Renal Association – European Dialysis and Transplant Association. ERA-EDTA History Stanley Shaldon www.era-edta.org/page-3-14-132-132-stanleyshaldon.html – accessed 14 June 2014; Brit Med J 2014; 348:27; Lancet 2014; 383: 508; Nephrol Dial Transplant (2014); 29: 467-469]