CKD Classification
A patient is said to have chronic kidney disease (CKD) if they have abnormalities of kidney function or structure present for more than 3 months.
The definition of CKD includes all individuals with markers of kidney damage (see below*) or those with an eGFR of less than 60 ml/min/1.73m2 on at least 2 occasions 90 days apart (with or without markers of kidney damage).
- *Markers of kidney disease may include: albuminuria (ACR > 3 mg/mmol), haematuria (of presumed or confirmed renal origin), electrolyte abnormalities due to tubular disorders, renal histological abnormalities, structural abnormalities detected by imaging (e.g. polycystic kidneys, reflux nephropathy) or a history of kidney transplantation.
CKD Classification
CKD is classified based on the eGFR and the level of proteinuria and helps to risk stratify patients.
Patients are classified as G1-G5, based on the eGFR, and A1-A3 based on the ACR (albumin:creatinine ratio) as detailed below:
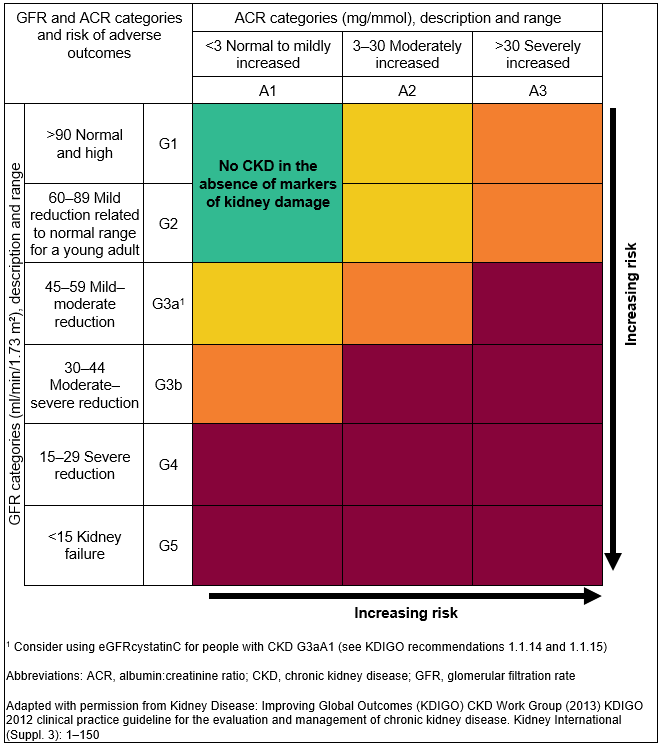
For Example
- A person with an eGFR of 25 ml/min/1.73 m2 and an ACR of 15 mg/mmol has CKD G4A2.
- A person with an eGFR of 50 ml/min/1.73 m2 and an ACR of 35 mg/mmol has CKD G3aA3.
It is important to note that patients with an eGFR of >60 ml/min/1.73m2 should not be classified as having CKD unless they have other markers of kidney disease (see above*).
Patient information
Patients with CKD can be classified depending on their level of kidney function, or eGFR, and the amount of protein present in the urine. This information forms the basis of CKD staging which is useful for planning follow up and management. The higher the stage (G1->G5) and the greater the amount of protein present in the urine (A1->A3) the more "severe" the CKD and the higher the risk that a patient may develop renal failure requiring dialysis in the future.
Kidney Failure Risk Equation (KFRE)
What is the Kidney Failure Risk Equation?
The Kidney Failure Risk Equation (KFRE) is a well-validated risk prediction tool for a kidney replacement therapy (KRT) in the next two or five years in individuals with chronic kidney disease (CKD) stages 3a-5.
To estimate the risk of KRT, the four-variable KFRE uses:
- Age
- Sex
- Estimated glomerular filtration rate (eGFR)
- Urine albumin:creatinine ratio (ACR)
The KFRE has been re-calibrated specifically for the UK population and is available via this website. Please note that this may be different from some other publicly available calculators.
When should the Kidney Failure Risk Equation be calculated?
The KFRE should be calculated when an individual with CKD Stage 3a-5 has an eGFR and ACR measured. This should be at least on an annual basis, but more frequently with more advanced disease (see the frequency of monitoring section of management of patients with CKD). We would recommend that both eGFR and ACR should be within six months of each other, and ideally within a month.
How will the Kidney Failure Risk Equation improve care for my patients?
-
The UK re-calibrated KFRE has recently been recommended by NICE to guide personalised care for people with CKD stages 3a-5 including referral to secondary care. If the risk of KRT is >5% in the next 5 years, referral should be considered factoring in the patient's 'wishes and comorbidities'. This threshold has replaced the previous recommendation for considering referral if eGFR is less than 30 ml/min/1.73m2. This is because it is likely to be more sensitive and specific for KRT and may reduce the number of people referred unnecessarily.
-
Two-year predictions may be more applicable to secondary care when discussing the risk of requiring KRT over a shorter timeframe and planning for procedures such as fistula formation or transplant listing.
How do I communicate Kidney Failure Risk Equation scores with patients?
Discussing KRT risk with should follow NICE's guidelines for 'shared decision making' and should include:
- Discussing KRT risk in the context of a patient's life, such as comorbidities and what matters most to the patient
- Describing KRT risk over the appropriate timeframe using 'natural frequencies' such as '10 in 100', instead of percentages such as '10%'
- Use a mixture of numbers and pictures
What are some limitations of the Kidney Failure Risk Equation?
- As KFRE uses eGFR and urine ACR to make a prediction, the same limitations for eGFR and urine ACR are also applicable to KFRE. Examples include assessment of patients at extremes of weight or muscle mass, or where a patient is being assessed in the context of acute kidney injury, or for ACR where a patient has a urinary tract infection. Please see the measurement of kidney function sections on eGFR and albuminuria for further explanation.
- KFRE should always be viewed in the context of the individual, their comorbidities, and their risk of dying from other causes over a period of the next two/five years.
- There has been limited specific validation of the KFRE in primary renal pathologies such as glomerulonephritis, cystic kidney disease and vasculitis. Therefore, in these groups caution should be used when making predictions based on KFRE.
More detailed information on KFRE including its development is available here.
Visit the UK validated KFRE website for more information
CKD Stages G1 and G2
Identifying patients with CKD stages G1 & G2
An eGFR of >90 ml/min/1.73m2 is considered normal kidney function. If these patients have evidence of kidney disease* however (see below) they should be classified as CKD stage G1.
Patients with an eGFR of 60-90 ml/min/1.73m2 have mildly reduced kidney function which may be appropriate for their age. If these patients have any other evidence of kidney disease* (see below) they have CKD stage G2.
*Evidence of kidney disease, required to diagnose CKD in patients with an eGFR >60 ml/min/1.7m2, may include:
- Proteinuria
- Haematuria (of presumed or proven renal origin)
- Structural abnormalities (e.g. reflux nephropathy, renal dysgenesis, medullary sponge kidney)
- A known diagnosis of a genetic kidney disease (e.g. polycystic kidney disease)
- Abnormalities detected by examination of renal histology
- Electrolyte abnormalities due to renal tubular disorders
- History of kidney transplantation
Initial assessment of CKD stages G1 and G2
The initial assessment for most of these patients will be undertaken in primary care settings.
The aim of the initial assessment is to determine which patients are at risk of progressive renal disease.
- All patients should have a urine specimen sent for measurement of the albumin:creatinine ratio (ACR).
- Urine reagent stick should be used to check for haematuria.
- If assessment is precipitated by a first discovery of an elevated serum creatinine level it is important to ensure that the renal function is stable. Previous blood tests, if available, will give you the answer. If no previous blood tests are available and the patient is well with no other worrying features (e.g. high potassium, symptoms of bladder outflow tract obstruction, severe hypertension), repeat the test within 14 days. Patients with deteriorating renal function require rapid assessment.
- Measure blood pressure. CKD can be a consequence of hypertension and CKD of any aetiology can be associated with hypertension. An elevated serum creatinine level may be the first clue that a patient is hypertensive.
Management of CKD stages G1 and G2
This applies to patients with stable stages G1 and G2 CKD. To diagnose CKD, two or more blood tests are required at least 90 days apart. The CKD staging and management outlined below is predicated on stable renal function.
Almost all patients with stages G1 and G2 CKD can be appropriately managed in primary care. The principal aim is to identify individuals at risk of progressive renal disease.
Some patients need further investigation where there are indications that progression to end stage renal failure (Stage G5) may be a possibility. These patients should usually be referred to the local nephrology service. Pointers to progression of renal disease include:
- Proteinuria - the risk is graded but a common cut-off for further investigation in patients without diabetes is ACR>70 mg/mmol or PCR>100 mg/mmol
- Haematuria of renal origin
- Rapidly deteriorating renal function
- Young age - the referral threshold should be much lower for younger patients in whom the lifetime risk of developing progressive kidney disease is higher.
- Family history of renal failure
- Hypertension which is difficult to control
Risk of cardiovascular events and death is substantially increased by the presence of CKD and or proteinuria and the risks of these two are additive. Patients with stages G1 and G2 CKD are much more likely to suffer a cardiovascular event than they are to require renal replacement therapy (dialysis or a transplant) in their lifetime. Patients should be offered lifestyle advice including recommendations for regular exercise, smoking cessation and attainment and maintenance of a healthy weight.
Long term monitoring of renal function, proteinuria and blood pressure should be performed for all patients. The principal aim of long term monitoring is to identify the minority of patients with stage G1 and G2 CKD who will go on to develop progressive renal disease.
- Renal function and proteinuria - patients with a urine ACR >3 mg/mmol (i.e. A2 and A3) should undergo annual monitoring of renal function and proteinuria. Patients with ACR<3 mg/mmol may be monitored less frequently (See more on stages of CKD). Patients with evidence of rapidly progressive renal impairment or who have worrying features (e.g. difficult to control hypertension, anaemia, hyperkalaemia, features of a systemic disease) should be considered for referral to renal services.
- Worsening proteinuria is an adverse prognostic sign. In patients with worsening proteinuria which exceeds ACR>70mg/mmol consider referral / discussion with nephrology unless it is known to be caused by diabetes and is appropriately treated. (See the management of patients with CKD section on Referral Guidelines).
- Blood pressure - Aim to keep the BP <140/90. In patients with CKD and diabetes or an ACR>70 mg/mmol aim to keep BP<130/80. (See the management of patients with CKD section on blood pressure (hypertension) management.)
- Cardiovascular disease - Offer advice on smoking cessation, exercise and lifestyle. (See the management of patients with CKD section on cardiovascular risk reduction.)
Patient information - CKD G1 and G2
CKD stage G1 is kidney disease with normal renal function. Patients with CKD stage G2 have mild impairment of kidney function. Most patients with CKD stages G1 and G2 just need occasional testing to ensure things are stable. A small minority of patients need further investigations to see if they have a disease which may benefit from treatment or could lead to more serious kidney damage.
CKD Stage G3
Identifying patients with CKD stage G3
Patients with CKD stage G3 (eGFR 30-59 ml/min/1.73m2) have impaired kidney function. These patients can be further subdivided based on their eGFR as follows:
- CKD stage G3a: eGFR 45-59 ml/min/1.73m2
- CKD stage G3b: eGFR 30-44 ml/min/1.73m2
Remember that eGFR is only an estimate of kidney function (more info on eGFR).
Creatinine and eGFR in an individual are usually quite stable. Deteriorating renal function needs rapid assessment. Note that the guidance on CKD staging and management outlined below are only applicable to patients with stable renal function.
Initial assessment of CKD stage G3
The initial assessment of these patients should be undertaken in the primary care setting for the majority of patients. The principal aim of the initial assessment is to identify individuals at risk of progressive renal disease.
If assessment is precipitated by a first discovery of an elevated serum creatinine level it is important to ensure that the renal function is stable. Previous blood tests, if available, will give you the answer. If no previous blood tests are available, and the patient is well with no other worrying features (e.g. high potassium, symptoms of bladder outflow tract obstruction, severe hypertension), repeat the test within 14 days. Patients with deteriorating renal function require rapid assessment.
- Clinical assessment - Consider obstruction in patients with prominent urinary tract symptoms or suggestive clinical findings (e.g. palpable bladder).
Is the patient well? Is there a history of significant associated disease? Consider referral if patient is unwell, a systemic disease process involving kidneys is suspected and / or supported by urinary abnormalities or other indicators.
- Medication review - are there any potentially nephrotoxic drugs or drugs that need dose alterations in patients with renal impairment? Remember non-prescribed and over the counter medications, e.g. NSAIDs.
- Urine tests: dipstick for blood and quantitation of proteinuria by ACR. Presence of haematuria or proteinuria may suggest intrinsic renal disease.
- Think if the CKD could be a complication of an existing diagnosis or a presenting feature of a new diagnosis e.g. diabetes, hypertension, multiple myeloma, connective tissue disease.
- Is there a family history of CKD or renal failure? May suggest a heritable disease, such as ADPKD, Alport's syndrome, reflux nephropathy.
- Imaging - exclusion of obstruction is indicated in patients with significant urinary symptoms or in whom there is a clinical suspicion of obstruction. An ultrasound scan of the renal tract is the usual screening investigation in this setting.
Management of CKD stage G3
This applies to patients with stable CKD stage G3.
Some patients need further investigation where there are indications that progression to end stage renal failure (Stage G5) may be a possibility. These patients should usually be referred to the local nephrology service. Pointers to progression of renal disease include:
- Proteinuria - the risk is graded but a common cut-off for investigation in patients without diabetes is ACR>70 mg/mmol or PCR>100 mg/mmol
- Haematuria of renal origin
- Rapidly deteriorating renal function
- Young age - the referral threshold should be much lower for younger patients in whom the lifetime risk of developing progressive kidney disease is higher.
- Family history of renal failure
- Hypertension which is difficult to control (on more than 4 agents)
Risk of cardiovascular events and death is substantially increased by the presence of CKD and or proteinuria and the risks of these two are additive. Patients with CKD stage G3 are, on average, more likely to suffer a cardiovascular event than they are to require renal replacement therapy (dialysis or a transplant) in their lifetime. Patients should be offered lifestyle advice including recommendations for regular exercise, smoking cessation and attainment and maintenance of a healthy weight. Offer patients with CKD stage 3-5 Atorvastatin 20 mg for the primary and prevention of cardiovascular disease and manage patients for secondary prevention as recommended by NICE.
Long term monitoring of renal function, proteinuria and blood pressure should be performed for all patients. The aims of monitoring are to identify the minority of patients with CKD stage G3 who will progress to end stage renal failure and to identify complications of CKD.
- Renal function should be monitored at least annually. For patients with significant proteinuria (i.e. A3) the renal function should be checked at least twice yearly. Consider referring patients to nephrology with rapidly declining renal function, i.e. a sustained decrease in GFR of 25% or more and a change in GFR category, or a sustained decrease in GFR of 15 ml/min/1.73 m2 or more within 12 months.
- Proteinuria - monitor with serial ACR or PCR. Note the suggested thresholds of ACR>70 (or PCR>100) mg/mmol for more stringent blood pressure targets and ACR>70 (or PCR>100) mg/mmol or ACR >30 (or PCR >50) mg/mmol with haematuria for specialist referral/discussion (see more on proteinuria in the measurement of kidney function section). Patients with diabetes and ACR>3 mg/mmol should be prescribed maximal tolerated dose of renin-angiotensin system inhibitors (RAASi) and sodium glucose co-transporter 2 inhibitors (SGLT2i). For non-diabetic patients with ACR>22.5 mg/mmol a SGLT2i should be considered. For non-diabetic patients with hypertension and ACR > 30 mg/mmol or ACR>70 mg/mmol (regardless of blood pressure) RAASi should be considered. (see more on RAASi and SGLT2i in the management of patients with CKD section).
- The 4 variable Kidney Failure Risk Equation (KFRE) should be used to calculate patient risk of progression to renal failure using age, sex, eGFR and urine ACR values every time renal function monitoring is undertaken. A 5-year risk of kidney failure >5% should prompt referral to a nephrology specialist. (see more on KFRE in the CKD stages section)
- Blood pressure - Aim to keep the BP <140/90. In patients with CKD and diabetes or an ACR>70 mg/mmol aim to keep BP<130/80 (see more on hypertension and blood pressure in the management of patients with CKD section).
- Cardiovascular risk - offer advice on smoking, exercise and lifestyle. Consider offering Atorvastatin 20 mg nocte for the primary and secondary prevention of cardiovascular disease (see more on cardiovascular risk reduction in the management of patients with CKD section).
- Haemoglobin - if low, first exclude "non-renal" aetiologies. Haemoglobin levels fall progressively commensurate with deteriorating renal function although significant anaemia attributable to CKD is rare before CKD stage G3b or G4. For patients with haemoglobin levels approaching or below 100 g/L specific interventions may be considered. (see more on anaemia in the complications of advanced CKD section).
- Immunisation - influenza and pneumococcal vaccination should be offered. Currently patients with CKD 3 are also being offered seasonal COVID boosters (subject to change)
- Medication review - regular review of medication to minimise nephrotoxic drugs (particularly NSAIDs) and ensure doses of others are appropriate to renal function.
Patient information
Patients with CKD stage G3 have impaired kidney function. Only a minority of patients with CKD stage G3 go on to develop more serious kidney disease. Cardiovascular disease, the umbrella term for diseases of the heart and circulation (e.g. heart attacks and strokes), is more common in patients with CKD. It is important to try and identify which patients may go on to develop more serious kidney damage and to try and reduce the chances of patients developing serious complications. It is important that blood tests are monitored regularly (6-12 monthly) to look for any significant decline. In addition to this it is essential that the level of protein in your urine (ACR) is also checked regularly, this can help us determine your risk (see kidney failure risk equation) and also your eligibility for important therapies that can reduce the likelihood of you developing serious kidney or heart disease.
CKD Stages G4 and G5
Identifying patients with CKD stage G4 and G5
Patients with an eGFR of 15-29 ml/min/1.73m2 have CKD stage G4 which represents significant impairment of kidney function.
Patients with an eGFR of <15 ml/min/1.73m2, or who require some form of dialysis, have CKD stage G5 which is often referred to as End-Stage Renal Failure (ESRF). This CKD stage represents patients with the lowest level of kidney function.
Creatinine and eGFR in an individual are usually quite stable. Deteriorating renal function needs rapid assessment. Note that CKD staging and management outlined below are only applicable to stable renal function.
Initial assessment of CKD stage G4
Initial assessment is identical to CKD Stage G3 but, in contrast to Stage G3, referral to or discussion with a specialist service will be usual. Exceptions to 'always refer or discuss' may include patients in whom:
- Severe renal impairment is part of another terminal illness.
- All appropriate investigations have been performed and there is an agreed and understood care pathway.
- Further investigation and management is clearly inappropriate.
If assessment is precipitated by a first discovery of an elevated serum creatinine level it is important to ensure that the renal function is stable. Previous blood tests, if available, will give you the answer. If no previous blood tests are available, and the patient is well with no other worrying features (e.g. high potassium, symptoms of bladder outflow tract obstruction, severe hypertension), repeat the test within 14 days. Patients with deteriorating renal function require rapid assessment.
In addition to referring these patients for specialist assessment in the majority of cases, patients should be evaluated with particular reference to the following points:
- Clinical assessment - If the patient is clinically unwell, consider telephoning for advice and to discuss expediting specialist assessment. Undertake an assessment of volume status (i.e. hypovolaemia - and hypervolaemia) and for symptoms or signs suggestive of renal tract obstruction (e.g. a palpable bladder).
- Medication review - any potentially nephrotoxic drugs, or drugs that need dose alterations when GFR reduced? Remember non-prescribed and over the counter medications, e.g. NSAIDs.
- Urine tests: dipstick for blood and quantitation of proteinuria by ACR/PCR. Presence of haematuria or proteinuria may suggest intrinsic renal disease (in contrast to pre- or post- renal disease).
- Blood tests: K+, Ca2+, Phosphate, Hb.
- Imaging - It is recommended to have a low threshold for performing an ultrasound scan in these patients to rule out a structural explanation and to provide additional clues about the aetiology and chronicity (i.e. renal size, cortical thickness, cortico-medullary differentiation). Consider requesting a scan urgently if there is a strong clinical suspicion of obstructive uropathy or prominent lower urinary tract symptoms. Consider requesting imaging at the same time as referring the patient for specialist assessment. (i.e. ordinarily referral to renal services should not be delayed pending the results of imaging studies).
Management of CKD stage G4 and G5
These patients should have a management plan that has been advised by a kidney specialist, either with an agreed management plan and a defined threshold for re-referral or under follow-up in a kidney clinic. The aims of management for patients with CKD stages G4 and G5 are to try and slow the progression of CKD, identify and treat the complications of CKD, reduce the incidence of cardiovascular disease, and to allow timely and informed decision making regarding the management of kidney failure.
Typically patients will be assessed, often through a combination of patient-clinician encounters and / or blood test, on a 3-4 monthly basis. The frequency of review will be determined by factors such as the rate of progression of CKD, KFRE, the patient's comorbidities, and the associated complications of CKD.
Factors which should be monitored and addressed in these patients include:
- Potassium levels - hyperkalaemia that is severe or not responsive to changes in therapy should lead to discussion or referral. Medications are often contributory in this setting.
- Bicarbonate level - bicarbonate levels fall as renal function declines. Sodium bicarbonate is often used in these patients.
- Haemoglobin – if low, exclude non-renal causes. Management of "renal" anaemia can include the provision of iron and the use of erythropoiesis stimulating agents. (see more on anaemia in the complications of advanced CKD section)
- Calcium and phosphate - Secondary hyperparathyroidism (SHPT) is frequently encountered in these patients. Management is multifaceted and can include dietary phosphate restriction and oral phosphate binders. Nutritional vitamin D (cholecalciferol) supplementation should be used where indicated, activated vitamin D (calcitriol or alfacalcidol) should be reserved for patients with SHPT that is severe or progressing towards severe.
- Urinary protein - monitor with ACR or PCR.
- KFRE
- Blood pressure - Aim to keep the BP <140/90. In patients with CKD and diabetes or an ACR>70 mg/mmol aim to keep BP<130/80. (see more on hypertension in the management of patients with CKD section)
- Cardiovascular risk - offer advice on smoking, exercise and lifestyle. Consider offering Atorvastatin 20 mg nocte for the primary and secondary prevention of cardiovascular disease. (see more on cardiovascular risk reduction in the management of patients with CKD section).
- Fluid Status- Salt and water retention is common in patients with impaired kidney function. Worsening of fluid retention may require initiation or up titration of diuretics and can precipitate the need to commence renal replacement therapy.
- Immunisation - influenza and pneumococcal vaccinations should be given. Patients who are likely to require renal replacement therapy should be vaccinated against hepatitis B. Seasonal COVID booster vaccinations are being offered to patients in this cohort.
- Medication review - regular review of medication to minimise nephrotoxic drugs (particularly NSAIDs) and ensure doses of others are appropriate to renal function. Metformin should be avoided in patients with CKD stage G4 and G5.
Patient information - CKD stages G4 and G5
Patients with CKD stages G4 and G5 have the most severe impairment of kidney function. Treatment of these patients involves trying to preserve kidney function and managing the complications that arise in patients with poor kidney function. These patients are also at very high risk of diseases which affect the heart and blood vessels, such as heart attacks and strokes. End-stage renal failure refers to patients who have insufficient kidney function to keep them feeling well and who may benefit from treatments which take on some of the functions of the kidney, such as dialysis or a transplant.