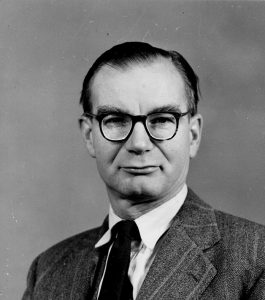
Eric Bywaters’ life spanned the growth of modern day rheumatology as a separate speciality of medicine. It was his early work as a teacher at the Postgraduate Medical School in Hammersmith that inspired much of that change.
At the age of 11 he won a scholarship to the Sutton Valence School in Kent, where his biology teacher interested him in collecting and making detailed drawings of rotifers, the microscopic free-swimming transparent animals with eyes, stomach and genitalia that live in puddles and streams. This interest in biology steered him to a career in medicine. He qualified from the Middlesex Hospital Medical School in 1933 with a gold medal and honours in pathology. He was appointed as assistant pathologist to Lionel Whitby [Munk’s Roll, Vol.V, p.444]. While researching on cartilage with Sir Charles Dodds [Munk’s Roll, Vol.VI, p.151] at the Courtauld Institute he came to the notice of Walter Bauer, a pioneer of rheumatology in the USA, who invited him in 1937 to Harvard at the Massachusetts General Hospital. There he studied patients with lupus erythematosus; his wife, Betty, doing the follow-ups.
In 1939, when war was imminent, they returned to London, but Bywaters was rejected for military service because of a kidney problem. He took over the rheumatism clinic at the British Postgraduate Medical School in Hammersmith Hospital, setting up a study of the life history and clinical outcome in 200 patients with rheumatoid arthritis. When the bombing of London started, he studied casualties whose limbs had been trapped by falling masonry and who after rescue developed fatal kidney failure, a sequence that became known as the ‘crush syndrome’. In 1944 this work moved to Newcastle at the Medical Research Council Shock Research Unit. The cause of crush syndrome, he found, was the release into the blood stream from damaged muscles of the muscle protein, myoglobin. This blocked the tiny ducts in the kidneys so that urine and waste products could not be filtered from the blood. Bywaters used animal models to show that alkaline fluids by mouth or intravenously, if given in time, could keep the patient alive until the kidneys could heal. He was the first to introduce the Kolff artificial kidney to the UK for those with established kidney damage.
Before the war rheumatology was not a recognised speciality of medicine like neurology or cardiology. Indeed many teaching hospital physicians regarded arthritis patients as ‘bed-blockers’ who could neither be cured nor discharged from hospital. Such patients were referred to the physical medicine departments of hospitals, to spa hospitals at Bath, Buxton, Droitwich and Harrogate, or in London to outpatient clinics established by the Red Cross. Some consultants who believed in the theory of focal sepsis as the cause of rheumatic conditions injected patients with vaccines made from their own resident bacteria, a treatment that persisted long after its value was debunked. It fell to Bywaters and a few of his contemporaries to change these attitudes and practices.
After the war the possibilities for research into the rheumatic diseases were greatly increased by the introduction of the free National Health Service in 1948 and funding became increasingly available from the Empire Rheumatism Council, the Medical Research Council and the Nuffield Foundation.
In 1947 Bywaters had taken on the additional responsibility of director of the special unit for juvenile rheumatism at the Canadian Red Cross Memorial Hospital at Taplow, near Maidenhead. Built on part of the Cliveden estate, it had been a military hospital in the First World War. In the Second World War it was leased by the Astors to the Canadian Red Cross as a hospital for the Canadian forces. When the war was over the hospital buildings were offered to the UK Government for research and treatment of rheumatic fever in children. A hospital purely for rheumatic fever was not practical, so it became a small general hospital with three of its 30 bed ward units devoted to the special unit. One other ward was converted to offices and research laboratories. There was meticulous follow-up of the patients organised through outreach clinics at Slough, Isleworth, Reading, Hammersmith and the National Heart hospitals.
When Hench and Kendall described the seemingly miraculous effects of cortisone on arthritis in adults in 1948, the special unit was poised to take part in a combined US/UK study of the effects of the hormone in rheumatic fever children. The immediate and dramatic effects of cortisone on their painful inflamed joints were confirmed but the important question was ‘did cortisone protect the heart from rheumatic heart disease?’ The answer after five years, disappointingly, was that it did not. Nevertheless, the introduction of powerful antibiotics and the general increase in post war public hygiene were able to prevent and cure the streptococcal infections that triggered rheumatic fever. By 1960 new admissions for rheumatic fever were a rarity and most young doctors then in training would never see the disease. The clientele of the special unit changed from rheumatic fever to juvenile forms of chronic arthritis, previously known as Still’s disease.
Bywaters’ forte was in his expertise in pathology and in his visual approach to the rheumatic diseases. He explored these from the clinical to the ultramicroscopic level, often enlisting new methods of imaging to make a research point or a more telling teaching slide. He left to others in his team the molecular intimacies of auto-immunity, which most rheumatologists accept as the most likely cause of the inflammatory rheumatic diseases. He used his skill in pathology to clear up ambiguities of diagnosis, firmly differentiating rheumatic fever from rheumatoid arthritis at tissue level. Others consulted him for his expertise in the morbid anatomy and tissue pathology of the rheumatic diseases. Some of his patients left him their spines for research. His last observations based on dissections of the spine in ankylosing spondylitis were published when he was aged 90. He was also a pioneer in the study of bone diseases, introducing an early method of quantifying osteoporosis and showing how other bone conditions could affect joints.
At Hammersmith he continued his survey of 200 patients with rheumatoid arthritis seen early in their disease and followed them for 20 years, a study that yielded a wealth of material and became the basis for numerous studies of the natural history of the disease and the causes of death. He received the prestigious Gairdner award in 1968.
The habit of collecting, classifying and filing illustrative material had been with him since boyhood. With the help of his colleagues in pathology (and secretaries to do the filing) he collected microscope slides of the rheumatic lesions in those of his patients who died and photographs, x-rays and extracts of the case notes of those who did not.
He was an avid medical historian, amassing a lifetime collection of books and artefacts related to the history of rheumatic diseases, much of which he has donated to the College library and the library of the Wellcome Institute.
Perhaps he will be most remembered for his pioneering work on juvenile chronic arthritis. With the help of his colleagues, particularly Barbara Ansell, the management of these children was transformed. Whereas at one time they would be put to bed for long periods, their muscles wasting, their limbs stiffening in the position they were nursed in bed, it was Bywaters’ policy to use pain control with drugs and hydrotherapy and, if necessary, surgery in order to maintain or regain movement. Much of the work was of a ‘salvage’ nature in neglected children. His surgeon colleagues were the first to develop custom-made artificial hips for children. Other prosthetic joints followed; sometimes four or more joints had to be replaced. Inflammation of the eyes caused by the disease could lead to cataracts and blindness: ophthalmologists at Taplow found ways to counter this. Dentists had to devise ways of getting stiffened jaws to open and anaesthetists ways of administering anaesthetics to children with stiff necks. The body of expertise built up at Taplow spread out to the country as a whole. There are children, now grandparents, who but for Taplow would have perished. Based on the work at Taplow, paediatric rheumatology has today become a recognised specialty of its own.
Bywaters would like to be remembered for ‘seeding’ rheumatologists and rheumatology expertise throughout the world. Postgraduate students came to Hammersmith and Taplow in large numbers from the United Kingdom and the former colonies, 33 from Canada alone, and almost as many from Australia and New Zealand. But many came from Europe (Greece, Yugoslavia, Holland, Egypt). Some of them became professors in their own universities, spreading knowledge wider. Bywaters counted 349 trainees over his period of service and he was later able to visit many of them in their own countries and universities. He was also proud of his contribution in bringing the medical perception of rheumatology firmly into the orbit of general medicine.
He started painting in watercolours during the First World War, when he was evacuated to Southsea. He began painting in oils later and became a skilled portrait artist. He went into caricature as a medical student when he was editor of the hospital magazine (tolerated, usually, by his teachers). He regularly caricatured himself and family in annual Christmas cards: the collection of these forms a visual history of his life and times. He studied the work of artists suffering from rheumatic diseases.
He was a keen gardener and a member of the Royal Horticultural Society. He was proud of his rare ‘Union Jack’ dahlia (petals arranged as alternate red and white stripes) that had been acquired as a tuber from Eleanor Singer, in Suffolk, to whose house his wife and family had been evacuated towards the end of the war. In his Beaconsfield garden there stands a platanus orientalis that he grew from a seed from the original plane tree under which Hippocrates is said to have taught. After his wife Betty died in 1998 he found the garden a great consolation.
Bywaters, who outlived most of his contemporaries, saw many changes in rheumatology. Before the war, and for ten years after, rheumatic fever was a common condition, killing many. Today it has disappeared. Today no one need suffer from gout. Prosthetic replacements for hip arthritis have become common and routine. Although rheumatoid arthritis still resists attempts at prevention and cure, the outlook for sufferers is now vastly better than it was 60 years ago. Drugs that cure pain and inflammation are safer and more effective. Genetic engineering holds out strong hopes of finding a cure. But new perils threaten as tuberculosis and other infections that can invade joints and bones are returning on the back of the AIDS pandemic.
Note by RA Archivist
For nephrologists, Bywaters’ name is inextricably bound with his seminal observations about crush syndrome in people trapped under buildings during the Blitz in London in World War II. It is hard to believe that such far-reaching observations, which led the way in establishing a pathophysiological basis for our understanding of acute renal failure, were just a brief interlude in the career of a rheumatologist. A rheumatologist who, as the obituary above (written by a rheumatologist) reminds us could equally well be remembered for transforming the care of children with juvenile arthritis. Remarkable achievements both.