My fistula and me
Steve, home haemodialysis patient
Me and my fistula have had a pretty complicated relationship. Initially, I didn’t want one, but then reluctantly agreed to have one made in December 2017. I switched from PD and started needling in March 2018. At first I was embarrassed about the tell-tale lumps and bumps but now I display them proudly. They represent my lifeline and when people ask about them it’s all the opportunity I need to talk about Kidney Disease and Dialysis.
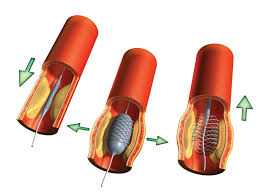
Sadly my fistula is prone to stenosis (blockages) that grow really close to the anastomosis (the physical join of the vein and artery). This often leads to fistula-plasty where essentially a balloon is placed at the point of the narrowing and inflated to stretch the vein and clear the obstruction.
In the last 3 years I’ve had 6 fistulaplasty and they’ve all reinstated good flow to my fistula and the process of monitoring has restarted. That was until Wednesday 13th January…
As normal I was at the hospital for 8.00am and the same doctor that had done my previous procedures set about his business. A few hours later my wife came for me and home I went.
I do my Home HD on alternate nights , 8 ½ hours at a time and I’d juggled my rota so that Wednesday 13th was a night off, because I wanted things to settle a little before I used the fistula for Dialysis.
On Thursday I was conscious that my forearm was more tender than it had been previously and a little swollen. When I came to hook up at bedtime I couldn’t get a ‘flash’ of blood – in fact I couldn’t get blood at all, despite several attempts at repositioning the needle. I assumed I was hitting swelling. As I’m generally pretty well I decided I could cope with missing the nights treatment and I’d try again the next night ( Friday) – surely another days recovery would only help?
Plans A to E
At lunchtime the next day I called my nurse, Kate, to let her know what had happened and what my plan was. Kate overruled me - she wanted me hooked up ASAP and I was to phone her immediately if I struggled again.
I set up and tried the first needle – 4 attempts to position the needle and still no ‘flash’. I rang Kate and she came straight round (I’m lucky she lives only a couple of miles away and was working at home). Kate had no more luck – it seemed to be all clot and no blood-flow. Whilst I assumed it was because of post-op swelling, Kate was much more concerned about the condition of my fistula and with the help of her colleague arranged an urgent scan for me, took blood samples and had me pack a bag as she thought there was little chance of me coming home that evening. The Doppler scan confirmed Kate’s fear, the fistula had clotted and I was in the hospital for the weekend.
On Saturday morning (16th) the only renal consultant in the hospital I’ve not met before was at my bedside, (I’ve now got the full set) I’d had no dialysis since Tuesday night and his hope was that I could get to Monday morning when they could attempt to angio-jet to remove the clotting and revive the fistula. Plan B was that I could have a tunnelled central line put in on Monday. If I couldn’t last till Monday, plan C meant I’d need a temporary neckline inserting later in the day, then the angio-jet on Monday which would then be re-labelled plan D and the tunnelled line would become Plan E. To inform the decision making yet more bloods were to be tested at lunchtime.
In my mind I was feeling well at the beginning of the week, bloods were great and there was no way having only missed two treatments that I couldn’t wait until Monday.
I was very very wrong.
My blood results made for shocking reading and I could feel the ‘dialysis fog’ returning.
There was little option, I needed dialysis to bring the potassium and other toxin levels down. Late on Saturday afternoon in went the temporary neckline, then I was connected for 4 much needed hours of dialysis

I’d seen temporary neck lines in use before, they looked to me really uncomfortable and even though I had been scared of needles, I was more scared of having a neckline. This was the moment I’d done everything I could to avoid – dialysis through a neck line.
On Monday morning (18th) I was back into theatre for the angio-jet. The doctor worked hard and eventually I heard him say to someone, ‘There it is - we’ve got flow’ the relief was immense – everything was going to be ok and the pain/discomfort/stress of the last few days could be washed away. The doctor set about removing whatever he put in my arm, and as he did it the fistula clotted again. I heard ‘no, we’ve lost it again’. I was overwhelmed, the anaesthetist noticed I was in tears and asked where the pain was - ‘between my ears’ was as much as I could give him.
They worked on and twice more they managed to get flow, but twice more it clotted before the equipment was withdrawn. Eventually defeat was conceded – my fistula was history.
From theatre I went up to dialysis and had another 4 hour treatment, to bring the toxin levels down and on Tuesday morning (19th) I was to be first into theatre for a tunnelled central line.
My journey back to home and independent dialysis
Several hours later I was home, with a plan in place for ongoing dialysis, back in centre on a Mon-Wed- Fri afternoon slot while I got some training on how to use and care for the new access, which wasn’t ideal as I’d previously been shielding away at home safe from COVID in my own little bubble.
While I was having my treatment on Wednesday 20th Kate, my home therapies nurse came to see me – she had a proposal, if I was happy to fit my treatment round her schedule over the next couple of weeks and be flexible over the length of treatment I got from session to session she’d come and train me at home – too good a deal to refuse so I began my home training on Friday 22 January.
Training for me needed to be tweaked from the standard package into a safe procedure I could manage on my own in my treatment room. The techniques need to be much ‘cleaner’ than those I was used to for self-cannulating my fistula due to the permanent route into the blood stream the tunnelled catheter could provide.
After the second run through at home the following Monday (25th January) we sat and wrote an agreed procedure/checklist that works for me in my space. Kate came 4 time that week, and I had 18 hours of treatment – I could feel the improvement in that ‘dialysis fog’. The following week she came again the first 3 working days. With each passing day I was becoming more proficient, and making fewer mistakes.
On the Wednesday (3rd February) Kate just observed, never interrupted or corrected, and she was satisfied that after 8 training session I was competent enough to dialyse unsupervised. From Friday I was flying solo again!
I’ve now done a few solo runs, I’m confident in what I’m doing but still reliant on my checklist. We’ve broken the list into 3 areas: setting up and preparation, cleaning and finally connecting. Of course I haven’t had to learn to use the machine as I’m already proficient in that.
It’s my plan to return to nocturnal treatment in a few weeks, once I’ve reached a level where I don’t need the checklist and the procedure is instinctive so that I can react to any issues without needing to fumble for my list. The tunnelled catheter is much less intrusive than I thought it would be and the connection procedure was no more difficult to learn, although for my lifestyle, I’m hoping to have a new fistula formed further up my arm so that I can resume taking my grandchildren swimming, which I’m not able to do with the central line in place.
Looking back, it was a difficult week, but I’ve had other difficult weeks before and I’m sure there are others to come.
What this experience has taught me
What I have learned (or had reinforced) is that all problems need to be communicated to your nurse – I’m so thankful I made the call to tell Kate I’d had a problem following my fistula plasty – but even that morning delay in contacting her almost made us run out of time for getting sorted with scans and blood tests and I’m so grateful to her for the care and attention she gives me.
I’ve also learned that despite feeling great most of the time, I’m just 2 missed sessions away from having dangerously high toxin levels with all the risks that brings.
I’m 2 weeks over it now and thankfully toxins have been lowered to a much more acceptable level and once I’m back on nocturnal I’m sure they’ll be back to what we consider ‘normal’ for me.